試管嬰兒已經進入PGS第三代,
第一代是第三天胚胎切片用螢光原位雜交染色法FISH,因為只有看5個、9個染色體,而且第三天胚胎切片,經由美國紐澤西RMANJ團隊,第三天切片一些會減少39%的胚胎著床率,
PGS第二代是第五天囊胚期胚胎切片,用aCGH也就是微陣列基因晶片,一來第五天切片不傷胚胎,著床率不會受影響,
第五天可以使用的胚胎分析還有SNP單核甘酸多樣性,
和最新的qPCR 3小時,
準確性多達98%,
但SNP時間比較久要24小時,
array CGH目前台灣要2到3天久的話要一個禮拜,國外可以12小時,
因此要冷凍胚胎,在美國紐澤西RMANJ團隊,直接跳過array CGH不用aCGH
他們專利的qPCR -- 24只要3小時有報告,準確率98%,根據Treff崔夫的設計不用96個探針,80幾個探針就可以偵測全基因24染色體,達到CCS;可以新鮮胚胎植入超快速,準確率98%,但有小小的缺點是微片段基因的缺陷抓不出來,
而array CGH一下去就是65萬個探針,平均每個染色體有2500到2700探針,解析度雖高,但有時候會太高,會誤殺胚胎,
第3代的PGS是次世代定序NGS,有三大特色:
(1)全基因診斷、
(2)單基因疾病診斷、
(3)細胞質的粒線體基因診斷,
目前英國針對吵的沸沸揚揚,3個爹娘試管嬰兒其實可以透過次世代定序NGS就可以免去三爹娘試管嬰兒的偵測。
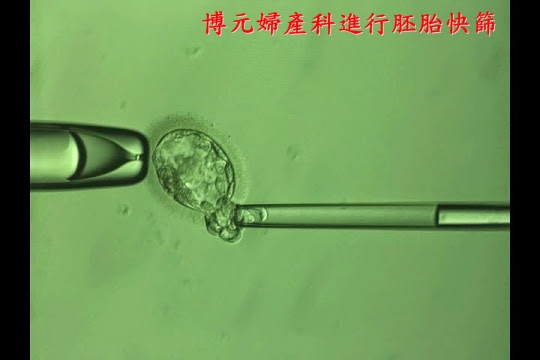
博元婦產科非常有負責的告訴妳:我們已進入PGS第2代的qPCR一條龍的試管嬰兒,我們的PGS不用冷凍胚胎,從打排卵針,取卵,培養囊胚,今天切片,今天或明天就有胚胎染色體報告可以植入健康胚胎,
我們的統計成績已發表在台灣婦產科醫學會年會,
qPCR的好處是:
(1)便宜、
(2)快速、
(3)準確率98%
(4)新鮮胚胎植入,免去冷凍胚胎的費用、
(5)省去妳煎熬等待當父母的漫漫長夜時˙間。
博元試管嬰兒中心以讓父母
少壓力、
少負擔、
少花費,
最快速度達到一圓子望求子的目的,
我們的終極目標是一次植入一個健康的寶寶,
也希望能夠一次成功,
在此告訴妳博元婦產科已經進入PGS第2代正邁向第3代的路上,妳還再冷凍胚胎做CCS嗎?妳還再冷凍胚胎嗎?美國紐澤西RMANJ團隊在最近一次生育與節育期刊發表7個理由,論述胚胎切片全基因檢查應該要新鮮植入胚胎的是世代已經到來見以下言文,
你還在冷凍胚胎苦等報告嗎?妳還再繳冷凍胚胎的費用嗎?
參考:
Comprehensive chromosome screening with
synchronous blastocyst transfer: time for a
paradigm shift*
Recently, the nature of assisted reproductive technology
(ART) laboratory investigation has been shifting. Tradition-
ally, it has focused on optimizing the culture milieu or assur-
ing fertilization; now, a variety of new technologies are
available to assess the reproductive potential of individual
embryos. Perhaps most prominent has been the resurgence
of embryonic aneuploidy screening. The validation of
24-chromosome testing platforms has led to a variety of
studies demonstrating higher implantation and delivery rates.
These findings are now translating to changes in the para-
digm of ART practice.
Caution is prudent in times of change, and methodical
analyses are needed. Evaluation logically focuses on efficacy
in terms of enhanced implantation and delivery rates. Other
factors, such as safety, cost, and accessibility also deserve
thoughtful consideration. Evaluations of these endpoints
should take into account the caliber of the data supporting
the ‘‘new paradigm,’’ in parallel with the data supporting
the current ‘‘standard of care,’’ and both should be evaluated
with the same level of rigor.
Several investigators have recently expressed concerns
about the implementation of comprehensive chromosomal
screening (CCS) in clinical practice. Fortunately, an ever-
growing literature is available to provide clinicians and scien-
tists with the information they need to evaluate many of the
critical issues. Some of the major issues and questions
include:
1. Efficacy of 24-chromosome embryonic aneuploidy
screening. Multiple studies provide class I data demon-
strating higher implantation and delivery rates following
24-chromosome aneuploidy screening. In distinct contrast
to fluorescent in-situ hybridization-based preimplantation
genetic screening studies in which every randomized
controlled trial (RCT) showed either no improvement or
active detriment, every RCT involving 24-chromosome
screening has demonstrated benefit (1–3).
2. What magnitude of improvement in clinical outcomes is
necessary to justify screening? Answering this question
inevitably involves a subjective decision that will be
made by patients after counseling by the clinicians caring
for them. Given that aneuploidy rates vary from 25% in
women in their late twenties to 85% for those in their
mid-forties, the opportunity for enhancing outcomes will
be greatly affected by the age of the female partner and
her intrinsic ovarian responsiveness. It is unlikely that im-
provements will be made in direct proportion to the aneu-
ploidy rate, as many other factors affect delivery rates.
Women with high embryonic arrest rates are unlikely to
attain the full benefit of screening. Still, the magnitude of
the enhanced outcomes seen in the RCTs is substantial.
3. The cost of CCS may be burdensome. Although substantial
costs are associated with CCS, even in proportion, they are
* This is an open access article under the CC BY-NC-ND license (http:// would appear that this type of screening is appropriate
660 VOL. 102 NO. 3 / SEPTEMBER 2014
lower than the costs of additional ART cycles. A definitive
cost-effectiveness study has not been published to date.
Although enhanced delivery rates should translate to fewer
treatment cycles, that question must await more detailed
analyses before conclusions may be drawn. Additionally,
savings attributable to decreased pregnancy losses and the
care provided to ongoing aneuploid gestations would need
to be considered. Given that, and the impact on transfer or-
der discussed below, it is unlikely that cost effectiveness will
limit implementation of embryonic aneuploidy screening.
4. Implementation of CCS may actually increase the risk for
multiple gestations unless transfer order is reduced. That
very fact has already been established in a randomized
controlled trial (2). In fact, it is a mathematical certainty.
As implantation rates increase, if there is no decrease in
transfer order, then multiple gestation rates will inevitably
rise. However, it is not reasonable to assume that transfer
order would remain the same. For the first time, there are
class I data demonstrating eSET after CCS is as effective
as double-embryo transfer of unscreened embryos (2).
All prior RCTs comparing elective single-embryo transfer
(eSET) versus double-embryo transfer found poorer per-
transfer outcomes with eSET. If CCS is used, that is no
longer true. Equivalent delivery rates are maintained while
virtually eliminating the risk of twins. The paradigm using
CCS and eSET produced an average gain in birth weight of
approximately 650 grams. No other single intervention in
obstetrics has produced such a dramatic enhancement in
birth weight, which is known to be highly correlated
with the health of the child. Of course, the transfer of
two screened embryos would further increase pregnancy
rates, but at the cost of quite elevated twin rates; thus, it
should be discouraged. Armed with these data, utilization
of eSET in our program has risen from less than 6% to
approximately 60% over a 4-year interval.
5. Embryo cryopreservation is essential to the application of
CCS. This is an excellent point, as it is true in many, but not
all, programs. Analyses can be completed in as little as
4 hours, and several programs now have testing labora-
tories within their facilities. However, that may not be
necessary. Data from RCTs demonstrate equivalent deliv-
ery rates following the transfer of fresh or vitrified CCS
screened blastocysts (2). Furthermore, data now demon-
strate meaningfully better obstetrical outcomes in concep-
tions following the transfer of cryopreserved embryos.
6. Some subpopulations may not benefit from aneuploidy
screening. The studies to date have focused on infertile
normal responders. No class I data address the impact of
CCS in women who are low responders or have recurrent
pregnancy loss. An RCT to determine the impact of CCS
in women at risk for low response to gonadotropin stimu-
lation has been registered (NCT01977144) and is currently
underway. Within the general ART population, individuals
who might typically be considered candidates for two-
embryo transfer should be offered CCS. Given that the
eSET rate was 8.8% in the recently released 2012 Society
for Assisted Reproductive Technology (SART) data, it
Fertility and Sterility®
for very large numbers of patients. Even those patients
who desire eSET attain increased delivery rates if the
euploid embryos are selected for transfer. Although
many of these patients already have excellent delivery
rates, it is difficult to imagine a scenario in which the in-
creases in implantation rates seen in the RCTs done to
date would not be a compelling reason to screen.
7. The need to culture to the blastocyst stage to safely biopsy
embryos increases the number of futile cycles because of
embryonic arrest prior to blastulation. This issue is
extremely important and represents a widely held belief,

.jpg)
.jpg)
.jpg)
.jpg)