紐澤西RMANJ的 次世代定序NGS研究 nextgen CCS新鮮胚胎植入的時代已經來臨,而冷凍胚胎時代已經過去
2015.02.26
紐澤西RMANJ的 次世代定序NGS研究 nextgen CCS新鮮胚胎植入的時代已經來臨,而冷凍胚胎時代已經過去
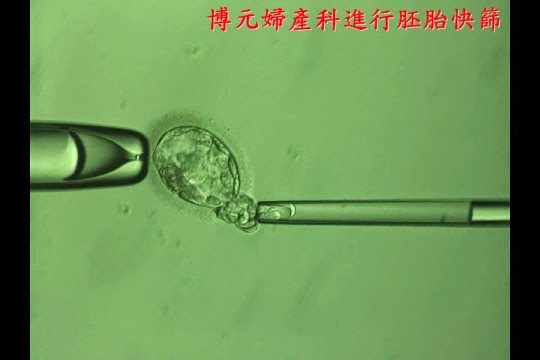.jpg)
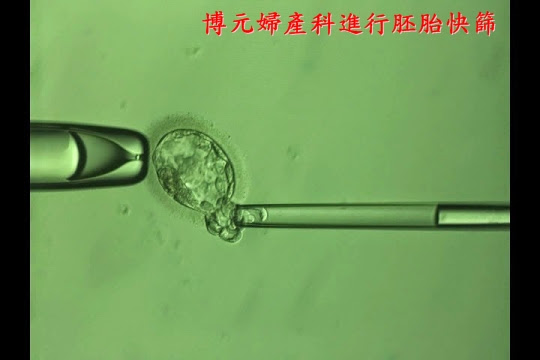.jpg)
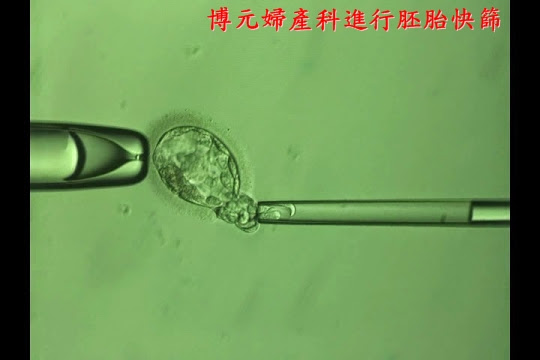.jpg)
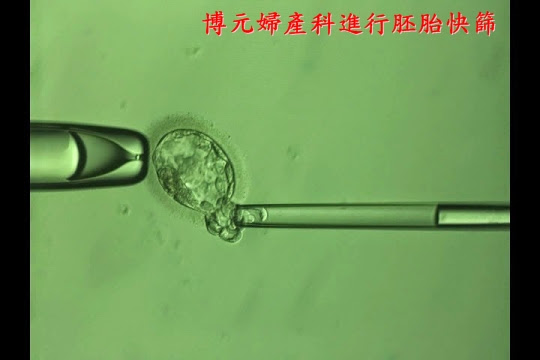.jpg)
在2014年去年2月10日首先RMANJ他們進行了一個200
這是一個雙盲的研究,實驗組是植入兩個經過次世代定序的胚胎,
而對照組是外觀選擇的胚胎,
次世代無疑它的好處是快速,
最重要的是很便宜,
在之前紐澤西團隊他們是是用qPCR來進行胚胎切片,獲得84.
他們仍然認為CCS應該可以
更精準或更便宜,
所以在去年2月進行了一個次世代定序的臨床研究,
有關RMANJ紐澤西團隊他們在1999年成立至今,
已經誕生3萬個試管寶寶,
在2013年美國生殖醫學會有發表28篇的學術論文,
他們最為人稱讚的是不斷的開發新的技術,
使用qPCR24染色體選胚胎植入胚胎:快速新鮮胚胎植入,
所以他們最近在美國不孕症與醫學期刊發表一份看法就是,
基於7個理由(ref):CCS新鮮胚胎植入的時代已經來臨,
RMANJ試管嬰兒中心更奇怪和有趣的觀察是,
他們不使用a-CGH去進行胚胎篩檢,
而從SNP跳到qPCR再跳到NGS,
而直接跳過a-CGH,
這真的很值得玩味的一個發現,是不是代表a-CGH:
(1)它在篩檢胚胎太過精準以至於會"誤棄"胚胎。
(2)會不會是太繁瑣要冷凍胚胎,
a-CGH的晶片費用非常的昂貴,
我們持續觀察美國紐澤西團隊次世代定序這200個研究NGS
應該會優於qPCR的84.7%的活產率 報告。
REF::
CCS不必冷凍胚胎,如王寶釧苦守寒窰18年等報告!qPCR
CCS 新鮮胚胎植入的 "7大" 理由,根據RMANJ紐澤西團隊斯考特Scott的論述,
(1)
(2)提高試管嬰兒成功率是最大的考慮,
(3)因為CCS的費用實在是很昂貴,
(4)使用CCS可以減少多胞胎的比率,
(5)冷凍胚胎其實是不可以不用的,
(6)有一些病人並不能從CCS得到好處,只有部分的病人,
(7)能夠進行CCS一定要:
1.進行囊胚期胚胎培養、
2.能夠進行胚胎切片、
3.能夠進行快速冷凍的方法。
因此這三大要件都存在的實驗室,才能夠進行CCS新鮮胚胎植入,
也因此
進行胚胎全基因放大檢測胚胎的染色體,
進行胚胎的植入"新鮮"胚胎植入,
參考:
Comprehensive chromosome screening with
synchronous blastocyst transfer: time for a
paradigm shift*
Recently, the nature of assisted reproductive technology
(ART) laboratory investigation has been shifting. Tradition-
ally, it has focused on optimizing the culture milieu or assur-
ing fertilization; now, a variety of new technologies are
available to assess the reproductive potential of individual
embryos. Perhaps most prominent has been the resurgence
of embryonic aneuploidy screening. The validation of
24-chromosome testing platforms has led to a variety of
studies demonstrating higher implantation and delivery rates.
These findings are now translating to changes in the para-
digm of ART practice.
Caution is prudent in times of change, and methodical
analyses are needed. Evaluation logically focuses on efficacy
in terms of enhanced implantation and delivery rates. Other
factors, such as safety, cost, and accessibility also deserve
thoughtful consideration. Evaluations of these endpoints
should take into account the caliber of the data supporting
the ‘‘new paradigm,’’ in parallel with the data supporting
the current ‘‘standard of care,’’ and both should be evaluated
with the same level of rigor.
Several investigators have recently expressed concerns
about the implementation of comprehensive chromosomal
screening (CCS) in clinical practice. Fortunately, an ever-
growing literature is available to provide clinicians and scien-
tists with the information they need to evaluate many of the
critical issues. Some of the major issues and questions
include:
1. Efficacy of 24-chromosome embryonic aneuploidy
screening. Multiple studies provide class I data demon-
strating higher implantation and delivery rates following
24-chromosome aneuploidy screening. In distinct contrast
to fluorescent in-situ hybridization-based preimplantation
genetic screening studies in which every randomized
controlled trial (RCT) showed either no improvement or
active detriment, every RCT involving 24-chromosome
screening has demonstrated benefit (1–3).
2. What magnitude of improvement in clinical outcomes is
necessary to justify screening? Answering this question
inevitably involves a subjective decision that will be
made by patients after counseling by the clinicians caring
for them. Given that aneuploidy rates vary from 25% in
women in their late twenties to 85% for those in their
mid-forties, the opportunity for enhancing outcomes will
be greatly affected by the age of the female partner and
her intrinsic ovarian responsiveness. It is unlikely that im-
provements will be made in direct proportion to the aneu-
ploidy rate, as many other factors affect delivery rates.
Women with high embryonic arrest rates are unlikely to
attain the full benefit of screening. Still, the magnitude of
the enhanced outcomes seen in the RCTs is substantial.
3. The cost of CCS may be burdensome. Although substantial
costs are associated with CCS, even in proportion, they are
* This is an open access article under the CC BY-NC-ND license (http:// would appear that this type of screening is appropriate
660 VOL. 102 NO. 3 / SEPTEMBER 2014
lower than the costs of additional ART cycles. A definitive
cost-effectiveness study has not been published to date.
Although enhanced delivery rates should translate to fewer
treatment cycles, that question must await more detailed
analyses before conclusions may be drawn. Additionally,
savings attributable to decreased pregnancy losses and the
care provided to ongoing aneuploid gestations would need
to be considered. Given that, and the impact on transfer or-
der discussed below, it is unlikely that cost effectiveness will
limit implementation of embryonic aneuploidy screening.
4. Implementation of CCS may actually increase the risk for
multiple gestations unless transfer order is reduced. That
very fact has already been established in a randomized
controlled trial (2). In fact, it is a mathematical certainty.
As implantation rates increase, if there is no decrease in
transfer order, then multiple gestation rates will inevitably
rise. However, it is not reasonable to assume that transfer
order would remain the same. For the first time, there are
class I data demonstrating eSET after CCS is as effective
as double-embryo transfer of unscreened embryos (2).
All prior RCTs comparing elective single-embryo transfer
(eSET) versus double-embryo transfer found poorer per-
transfer outcomes with eSET. If CCS is used, that is no
longer true. Equivalent delivery rates are maintained while
virtually eliminating the risk of twins. The paradigm using
CCS and eSET produced an average gain in birth weight of
approximately 650 grams. No other single intervention in
obstetrics has produced such a dramatic enhancement in
birth weight, which is known to be highly correlated
with the health of the child. Of course, the transfer of
two screened embryos would further increase pregnancy
rates, but at the cost of quite elevated twin rates; thus, it
should be discouraged. Armed with these data, utilization
of eSET in our program has risen from less than 6% to
approximately 60% over a 4-year interval.






